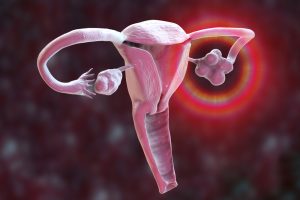
Most human eggs never have the chance to mature into eggs, a recent study sheds light on why. A new “atlas” of the human ovary provides insights that could lead to treatments that restore ovarian hormone production and the ability to have biologically related children.
Creating a Functional Follicle
This deeper understanding of the ovary means that researchers could potentially produce artificial ovaries in the lab, using tissue that has been stored and frozen prior to exposure to toxic medical treatments such as chemotherapy and radiation. Currently, surgeons can implant previously frozen ovarian tissue to temporarily restore hormone and egg production. However, this does not work for long, as only a few follicles – the structures that produce hormones and carry eggs – survive through reimplantation.
The new atlas reveals the factors that allow a follicle to mature, as most follicles atrophy without releasing hormones or an egg. Using new tools to determine which genes are expressed at the single-cell level in a tissue, a team of researchers has been able to pinpoint ovarian follicles that carry the immature precursors of eggs, known as oocytes. Now that the researchers know which genes are expressed in the oocytes, they can test whether interfering with these genes could lead to the creation of a functional follicle, according to Ariella Shikanov, U-M associate professor of biomedical engineering and corresponding author of the new study in Science Advances. In this way, an artificial ovary can be created that could eventually be transplanted back into the body.
Longer Fertility Window
Most follicles, known as primordial follicles, are dormant and located in the outer layer of the ovary, the cortex. A small proportion of these follicles are activated at regular intervals and migrate into the ovary, into a region known as the growth pool. Only some of these growing follicles produce mature eggs that are released into the fallopian tube. With the ability to control the development of the follicles and optimize the ovarian environment, the team believes that the engineered ovarian tissue could function much longer than unmodified implanted tissue. This means that patients would have a longer fertility window and their bodies could produce hormones that regulate the menstrual cycle and support muscle, skeletal, sexual organ and cardiovascular health for longer. The magic that the researchers are working towards is being able to bring an immature cell to maturity. But to do this, they need to know which molecules control this process.
The team used a relatively new technology called spatial transcriptomics to track all gene activity – and where it occurs – in tissue samples. This is done by reading RNA strands, which are like notes of the DNA strand, and provide information about which genes are currently being read. In collaboration with an organ procurement organization, the U-M researchers performed RNA sequencing of ovaries from five human donors. According to Shikanov, this was the first time that the researchers were able to specifically examine ovarian follicles and egg cells and perform a transcriptional analysis that allows them to see which genes are active.
The majority of ovarian follicles already present at birth never reach the growth pool and eventually self-destruct. With this new data, researchers can begin to understand what makes a good egg – what determines which follicles grow, ovulate, get fertilized and become a baby. U-M’s work is part of the Human Cell Atlas project, which aims to “create maps of all the different cells, their molecular properties and their location to understand how the human body works and what goes wrong in disease.” Shikanov, Li and U-M collaborators such as Sue Hammoud, U-M associate professor of human genetics and urology, are mapping other parts of the female reproductive system, including the uterus, fallopian tubes and ovaries.