There are numerous factors that make fertilization difficult or completely impossible. In many cases, the cause lies with the man. One of the most important parameters for successful conception is good motility of the male sperm. A negative lifestyle, illnesses, the use of certain medications, stress and advanced age can affect the quality of male sperm.
In fact, the sperm microbiome can also influence factors such as sperm motility. According to researchers from the Department of Urology at UCLA, the sperm microbiota may play a crucial role in influencing sperm parameters and improving male fertility.
How Certain Microbes Affect Male Fertility
In light of recent studies highlighting the importance of the microbiome to overall human health, researchers examined the sperm microbiome to understand its potential impact on male fertility.
The study found that one microbe in particular, Lactobacillus iners, could have a direct negative impact on male fertility. The researchers found that men who had more of this microbe were more likely to have problems with sperm motility. Previous research has shown that Lactobacillus iners (a Gram-positive, rod-shaped bacterium) can preferentially produce L-lactic acid, which can lead to a local pro-inflammatory environment that could have a negative impact on sperm motility. The authors of the study point out that there is already research suggesting a link between this microbe and fertility, but most of the literature relates to the vaginal microbiome and female factors. This is the first study to show a negative association between the microbe and male fertility.
The researchers also discovered that three types of bacteria from the Pseudomonas group were present in patients with both normal and abnormal sperm concentrations. The microbes Pseudomonas fluorescens and Pseudomonas stutzeri were more common in patients with abnormal sperm concentrations, while Pseudomonas putida was less common in samples with abnormal sperm concentrations. However, the results suggest that not every member of the same closely related group can affect fertility in the same positive or negative way. In other words, even closely related microbes do not always have the same direct relationship with fertility.
This research is consistent with findings from smaller studies and will pave the way for future, more comprehensive investigations to unravel the complex relationship between the semen microbiome and infertility. Studying the functions of microorganisms in sperm may pave the way for the development of treatments aimed at correcting problems with sperm parameters.
CatSper Deficiency Prevents Successful Conception
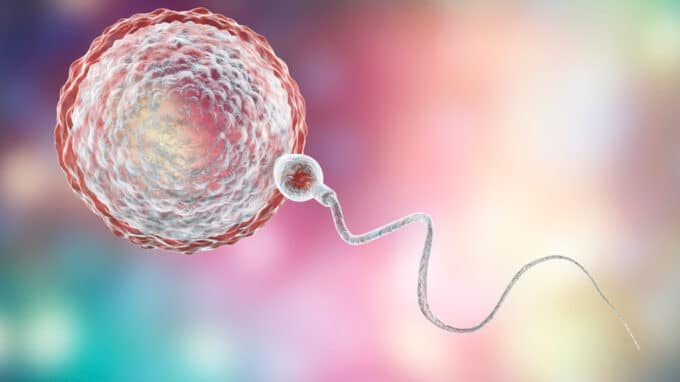
In about half of all couples who are unable to conceive a child, the infertility is due to the man. A new study identifies malfunctioning of “CatSper,” an ion channel that controls calcium levels in sperm, as a common cause of seemingly unexplained male infertility. Human sperm with CatSper deficiency cannot fertilize the egg because they cannot penetrate its protective shell. To date, this sperm channelopathy has not been detectable. Scientists from Münster have decoded the role of CatSper in infertility using a novel laboratory test that identifies affected men. The results of the study, published in The Journal of Clinical Investigation, could improve the diagnosis and care of infertile couples.
One in six couples fails to have a child. The underlying cause often remains unclear. In about a third of infertile couples, the man’s sperm analysis reveals no abnormalities with regard to the number, motility or morphology of the sperm. This poses a problem: the lack of a clear diagnosis prevents evidence-based selection of a treatment option. As a result, affected couples often experience unsuccessful treatments.
Why is it that men cannot father children despite normal sperm parameters? An interdisciplinary team of scientists from the University of Münster in Germany got to the bottom of this question. A few years ago, Strünker and colleagues demonstrated that sperm cells use CatSper as a sensor to detect messenger molecules released by the egg. These molecules activate CatSper, resulting in an influx of calcium into the flagellum and altering its beating pattern.
To investigate whether this is essential for fertilization, the researchers developed a simple laboratory test with which they were able to determine the activity of CatSper in the sperm of almost 2,300 men. This showed that around one in a hundred infertile men with inconspicuous sperm parameters actually had a loss of CatSper function. The most common cause is genetic variants in genes that code for one of the components of CatSper.
Sperm need the CatSper-mediated changes in the flagellar beat in order to break through the protective sheath of the egg cell. Another important finding of the study: CatSper-induced male infertility also includes the failure of medically assisted reproduction through intrauterine insemination, in which sperm are introduced into the uterus via a catheter immediately before ovulation, or classic in vitro fertilization (fertilization in a Petri dish). This is not surprising, as these treatments require the sperm to break through the egg membrane. Affected men/couples have only been able to conceive a child using the ICSI method, in which a sperm cell is manually injected into the egg.
The Role of Proteins in Male Infertility
Thanks to this comprehensive research project, the experts have now been able to identify and diagnose this channelopathy, enabling evidence-based treatment of the affected couples. This can minimize the medical risk for couples and maximize the chances of success. Sperm function is not only controlled by CatSper, but also by various other proteins. These are also the focus of the Clinical Research Unit (CRU326) “Male Germ Cells” funded by the German Research Foundation, which formed the cooperative framework for the current study. The overarching goal of the Münster researchers is to systematically elucidate the role of these proteins in (in)fertility in order to improve the diagnosis and care of affected couples.